Health
Lilly Plans To Cut Some Insulin Prices $44, Expand Cost Cap
Eli Lilly will reduce the price of some older insulins later this year and provide more patients with immediate access to a cap on the costs they pay to fill prescriptions.
The actions announced on Wednesday provide critical relief to some people with diabetes who can face annual costs of thousands of dollars for the insulin they require to live. Lilly’s changes come as lawmakers and patient advocates pressure drugmakers to address rising prices.
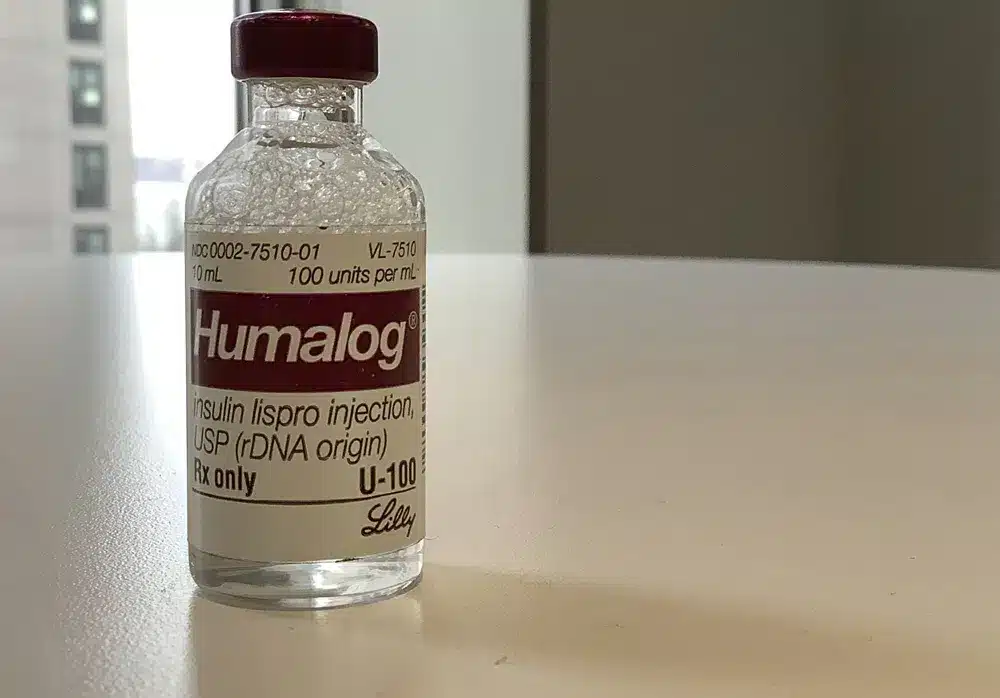
Lilly said it would reduce list prices for Humalog, its most commonly prescribed insulin, and Humulin, another insulin, by 70% or more in the fourth quarter, which begins in October.
List prices are what a drugmaker initially establishes for a product and what people without insurance or with high deductible plans are sometimes forced to pay.
According to a Lilly spokesperson, the current list price for a 10-mL vial of the fast-acting, mealtime insulin Humalog is $274.70. This will be reduced to $66.40.
Similarly, she stated that the same amount of Humulin is currently listed at $148.70. That will now be $44.61.
According to Lilly CEO David Ricks, the company is making these changes to address issues that affect the price patients ultimately pay for its insulins.
Lilly Humulin is currently listed at $148.70. That will now be $44.61
He noted that discounts Lilly offers from its list prices often only reach patients through insurers or pharmacy benefit managers. High-deductible coverage can result in large bills at the pharmacy counter, especially at the beginning of the year when deductibles renew.
“We know the current healthcare system in the United States has gaps,” he said. “This makes a difficult disease like diabetes even more difficult to manage.”
Patient advocates have long advocated for insulin price reductions to assist uninsured individuals unaffected by price caps tied to insurance coverage.
Lilly’s planned price cuts “could provide some substantial price relief,” according to Stacie Dusetzina, a Vanderbilt University health policy professor who studies drug costs.
She noted that the changes are unlikely to have a significant financial impact on Lilly because the insulins are older, and some are already competitive.
Lilly also announced on Wednesday that the price of its authorized generic version of Humalog would be reduced to $25 per vial beginning in May.
Lilly will also launch biosimilar insulin in April to compete with Sanofi’s Lantus.
Ricks stated that because insurers and the pharmacy system will take time to implement the price cuts, the drugmaker will immediately cap monthly out-of-pocket costs for people not covered by Medicare’s prescription drug program at $35.
According to the drugmaker, the cap applies to people with commercial insurance and at most retail pharmacies.
People without insurance, according to Lilly, can find savings cards for the same amount of insulin on its InsulinAffordability.com website.
In January, the federal government began applying that cap to patients with Medicare coverage, which is available to people 65 and older and those with certain disabilities or illnesses.
Last month, President Joe Biden mentioned the cost cap in his annual State of the Union address. He proposed capping insulin costs at $35 for everyone.
Lilly responded to Biden’s call, according to a statement released on Wednesday.
“It’s a big deal, and other manufacturers should follow,” Biden said.
He also stated that Americans have faced “far too long” and much higher drug costs than people in other countries.
Aside from Eli Lilly and the French pharmaceutical company Sanofi, Novo Nordisk is another insulin manufacturer.
Sanofi and Novo Nordisk representatives said their companies offer a variety of programs that help people with and without insurance save money.
The pancreas produces insulin, which the body uses to convert food into energy. Diabetes patients do not produce enough insulin.
To survive, people with Type 1 diabetes must take insulin every day. According to the American Diabetes Association, more than 8 million Americans use insulin.
According to research, insulin prices have more than tripled in the last two decades. Pharmaceutical companies are under increasing pressure to assist patients.
Lilly is trying to get ahead of the issue and appear to the public as the good guy,
California has stated that it intends to investigate the possibility of producing cheaper insulin. Drugmakers also may face competition from companies like the nonprofit Civica, which plans to produce three insulins at a recommended price of at most $30 a vial, a spokeswoman said.
Drugmakers may see “the writing on the wall that high prices can’t last forever,” according to Larry Levitt, executive vice president of the Kaiser Family Foundation, a nonprofit that studies health care.
“Lilly is trying to get ahead of the issue and appear to the public as the good guy,” Levitt said, adding that nothing prevents Lilly from raising prices again.
According to Lilly officials, they have not raised the prices of any of their insulins since 2017.
Lilly CEO Ricks stated that Wednesday’s changes were made “because it’s time and the right thing to do.”
In 1923, two years after University of Toronto scientists discovered insulin, Indianapolis-based Eli Lilly and Company became the first company to commercialize it. The drugmaker then built its reputation on insulin production, even as it expanded into cancer treatments, antipsychotics, and other medications.
Last year, Lilly earned more than $3 billion in revenue from Humulin, Humalog, and it’s authorized generic. The previous year, they made more than $3.5 billion.
“These are treatments that have a long and successful history and should be less expensive for patients,” Dusetzina said.
SOURCE – (AP)
Health
Kelly Clarkson Weight Loss Wasn’t Ozempic It Was a High Protein Diet
Kelly Clarkson’s remarkable weight loss has been a major topic of conversation for quite some time now, and the 42-year-old singer and talk show presenter has been very open about it with her fans!
The Kelly Clarkson program host had spoken up about her ever-shrinking figure multiple times, including on her talk program, when she admitted to utilizing a weight loss injection (not Ozempic!) to help her owing to being pre-diabetic.
Kelly revealed that she has lost a lot of weight, saying, ‘Mine is a different one than people assume, but I ended up needing to do it also because my blood work was so poor.’ She said that she had not taken Ozempic.
Kelly Clarkson did not name the medicine but described it as “something that aids in the breakdown of the sugar—my body does not do it right.”
She said her doctor ‘chased [her] for, like, two years’ to take the medication, but she was concerned about the consequences on her thyroid. However, she took it after seeing a birthday special she intended to release.
Kelly Clarkson Weight Loss
‘All of a sudden I halted it, and I was like, “Who the f*ck is that?'” she added. “You see it and you’re like, “Well, she’s about to die of a heart attack”,” Kelly said.
Whoopi, for her part, said she shed the weight of ‘nearly two people’ after ‘taking that great shot that works for persons who need some help.’
“It’s great for people like us who have issues,” the View co-host continued. She mentioned earlier that she is using Mounjaro for weight loss.
Her weight loss began following a health concern.
Kelly Clarkson originally hinted at her weight loss on her talk show, The Kelly Clarkson Show, in December 2023. According to US Today, she previously stated that she no longer wore Spanx. “It’s quite cold inside this building. I don’t even have to wear Spanx anymore. “I just wear them for warmth, like thermals,” Kelly explained during a singing game.
However, on January 29, Kelly said on her show that she was doing ‘ something’ about her weight after obtaining a pre-diabetic diagnosis a few years prior.
(According to the Centres for Disease Control and Prevention, pre-diabetes means having blood sugar levels that are ‘greater than usual’ but not high enough for a type 2 diabetes diagnosis.) ‘I wasn’t astonished,’ she explained. ‘I was a little bit overweight.
‘They said, “You’re pre-diabetic.” You’re right on the brink.” And I was like, “But I’m not there yet,” she added. ‘And then I waited two years and said, “Okay, I’ll do something about it.”‘
High Protein Diet
Kelly Clarkson has changed her diet and is focussing on consuming plenty of protein.
‘I eat a healthy mix,’ she told People. ‘I lost weight because I listened to my doctor, which I hadn’t done in a few years. And I succeed 90% of the time since a protein-rich diet already benefits me. I’m a Texas gal, so I enjoy meat—sorry, vegans of the world!”
Kelly stated that her diet is a ‘healthy mix’, which means she still allows sweets.
I still indulge. ‘The other night, I had frozen yoghurt with my daughter, and it was fantastic,’ she continued.
Kelly stated that in 2018 when on a weight-loss journey, she would change the ingredients in her meals to make them healthier. ‘It’s the same stuff you eat; I use different ingredients,’ she explained.
‘Even for fried chicken, I use cassava flour, tapioca, or almond flour, while you use hormone-free chicken.’
However, Kelly agreed that this is not the most convenient option for most people. ‘I’m going to be honest with you: it’s incredibly expensive,’ she said.
Kelly later stated that she had lost weight after reading Dr. Steven Gundry’s The Plant Paradox. The Plant Paradox Diet is lectin-free, excluding beans, legumes, whole grains, some vegetables, and dairy.
‘I literally read this book, and I followed it for an autoimmune condition and a thyroid issue, and now all of my numbers are back up,’ Kelly told Extra the same year. ‘Thanks to this book, I’m no longer taking medication. It’s all about how we cook our food: non-GMO, pesticide-free, and eating organically.
In addition to nutrition and exercise, Kelly revealed that she has been using infrared saunas, which have been shown to promote sleep, ease tension and pain, and help clarify skin.
She’s also tried cold plunges. ‘I just took a chilly plunge because everyone wore me down,’ Kelly explained.
Related News:
7 Causes of Eye Bags: Why You Look Tired
Health
MAID Now Accounts for 1 in 20 Deaths in Canada
Medical assistance in dying (MAID), often known as voluntary euthanasia, accounted for 4.7% of Canadian deaths in 2023, according to new Health Canada data.
According to Heath Canada’s fifth annual report, since the Trudeau government legalized MAID in 2016, about 15,300 persons will undergo assisted death in 2023 if their applications are granted.
The median age in this group was more than 77. The great majority, almost 96%, died from “reasonably foreseeable” causes, such as cancer.
In a tiny number of other cases, patients may not have been terminally sick but wanted assisted suicide owing to a protracted and difficult illness that had significantly reduced their quality of life.
Canada is one of a few countries that have passed assisted dying legislation in the last decade. Others include Australia, New Zealand, Spain, and Austria.
In Canada, consenting adults can request medical help in dying from a healthcare physician if they have a serious and irreversible medical condition. Some constraints exist, such as requiring two independent healthcare providers to certify the patient’s eligibility before the request is authorized.
Quebec Highest in MAID Deaths
In 2023, more than 320,000 individuals died in Canada, with medical assistance accounting for 15,300 of those fatalities (or around one in every 20).
According to estimates presented by Health Canada on Wednesday, the rate of assisted dying in Canada would rise by about 16% in 2023. This figure represents a significant decrease from the average increase of 31% in prior years.
The research stated that it is too early to determine what caused the rate to slow. For the first time, the report examined race and ethnic data on persons who received MAID.
Around 96% of receivers identified as caucasian, who comprise over 70% of Canada’s population. It’s unknown what produced the difference.
The second-highest reported ethnic group was East Asians (1.8%), who comprise approximately 5.7% of Canadians.
MAID remained the most commonly used method in Quebec, accounting for roughly 37% of all euthanasia fatalities despite the province’s population being only 22% of Canada.
The Quebec government initiated a study earlier this year to investigate why its euthanasia rate was so high.
Expanded Access to MAID
In 2021, the Trudeau government expanded access to MAID for persons who do not have a terminal diagnosis but wish to terminate their lives due to a chronic, disabling ailment. Earlier this year, it was announced that access to those with mental problems would be expanded again.
However, it was postponed for the second time because Canadian provinces, which control healthcare delivery, raised concerns about the system’s ability to handle such a large expansion.
On Wednesday, Health Canada defended the procedure, citing the criminal code’s “strict eligibility” conditions.
However, Cardus, a Christian research tank, claimed the latest MAID data were “alarming” and revealed that Canada has one of the world’s fastest-growing euthanasia regimes.
A report released in October by the Ontario government offered some insight on contentious cases in which people were awarded assisted dying when they were not reaching the end of their natural lives.
One example was a woman in her fifties with a history of melancholy and suicide ideation who was extremely sensitive to chemicals.
Her plea for euthanasia was granted after she was unable to find a home that could meet her medical requirements.
Another example made headlines recently, involving a Nova Scotia cancer patient who claimed she was twice asked if she was aware of assisted dying as an option while undergoing mastectomy surgery.
According to the National Post, the question “came up in completely inappropriate places”.
Many other Canadian news sites have also covered incidents in which people with disabilities considered assisted suicide owing to a lack of housing or disability assistance.
Related News:
BC Supreme Court Stops MAID Death of Woman from Alberta
Health
Diabetes Patients May Benefit From GLP-1 Medications
(VOR News) – Individuals with diabetes utilising GLP-1 medications, such as Ozempic or Mounjaro, may be gaining an additional benefit, as suggested by recent research findings. This advantage is a diminished probability of developing a potentially fatal blood clot.
The study’s findings revealed that diabetic patients on specific medications exhibited a twenty percent reduced risk of developing venous thromboembolism (VTE) compared to those on alternative diabetic treatments.
Dr. Rushad Patell, the principal author of the study, remarked that “from a public health perspective, considering the widespread use of these [GLP-1] drugs, there exists potential to ascertain whether the overall incidence of VTE could be diminished at a national or population level as a consequence of this study.”
This pertains to the prevalence of diabetes medications.
Given the escalating risk of venous thromboembolism (VTE), it is plausible that this will result in a shift of the curve in the contrary direction.
At the American Society of Haematology’s (ASH) annual meeting, which took place in San Diego on Sunday, his team gave a presentation of their research findings. The meeting took place in San Diego.
It is essential to keep these data in a preliminary form until they are published in a peer-reviewed publication because they were presented at a diabetes medical congress. At the convention, the results were presented.
The researchers highlighted that vein thromboembolism (VTE) is a prevalent clot formation in veins that can pose significant risks. The two predominant forms of venous thromboembolism are pulmonary embolism and deep vein thrombosis (DVT). Pulmonary embolisms are defined by the migration of blood clots to the lungs, whereas deep vein thromboses (DVTs) are defined by the formation of blood clots in the legs.
Any form of venous thromboembolism (VTE) can lead to hospitalisation and potentially death if left untreated.
Could the newly discovered GLP-1 diabetic medications, which have achieved significant market success, aid in the prevention of venous thromboembolism?
Over 558,000 individuals in the United States were registered in a comprehensive health care database, and Patell’s team monitored the outcomes of these participants to gather information regarding the circumstances.
Patients were categorised into two groups, each including roughly 279,000 individuals: those utilising a GLP-1 drug for diabetes control and those receiving an older class of diabetes medication referred to as DPP4i. Patients with comparable health conditions were divided into these two groups. DPP4 inhibitors, conversely, do not induce weight loss in the manner that specific GLP-1 medications do.
In comparison to the cohort receiving alternative diabetes treatment, the group administered GLP-1 therapy exhibited an average incidence of venous thromboembolism (VTE) of 6.5 per 1,000 patients after one year.
Clots per 1,000 patients in the alternative diabetes cohort were 7.9.
According to Patell and his colleagues, the risk of blood clot formation was diminished by twenty percent as a result of this. The occurrence of pulmonary embolisms and deep vein thromboses (DVTs) has been shown to be decreasing.
The researchers found that the patient’s obesity status before taking GLP-1 did not affect the advantages regarding clotting risk, which were consistent regardless of the individual’s weight. The ambiguity remains over whether the decreased clotting risk associated with GLP-1s is due to weight loss in individuals or if an alternative mechanism is involved. There is insufficient comprehension concerning this issue.
“Further studies are necessary to ascertain the potential mechanism, whether via weight loss or alternative methods,” Patell stated in a news release disseminated at an ASH convention: “We must identify the potential mechanism through weight loss.”
The study could not establish that the use of GLP-1s was the cause of the reduction in clotting due to its retrospective design. The study was conducted, which was the reason for this situation. Consequently, Patell and his associates have asserted that a prospective clinical trial is essential to validate the evidence reported to date. Patell asserts that the newly acquired data may still offer direction to individuals with diabetes and the medical experts who manage their care.
His hypothesis is that this finding implies potential advantages in choosing a GLP-1 receptor agonist as an antidiabetic drug for patients. He stated, “It is crucial to consider thrombotic risk when selecting an antidiabetic agent for a patient.”
SOURCE: USN
SEE ALSO:
Vesta Care Dubai: Transforming Healthcare with Personalized Home Services
Bird Flu Testing Mandatory For Milk Supply In Exclusive-US Issued Order
-
Politics4 weeks ago
Miller Expects 4.9 Million Foreigners to Leave Canada Voluntarily
-
News3 weeks ago
Nolinor Boeing 737 Crash Lands in Montreal
-
News3 weeks ago
“Shocking Video” Vancouver Police Shoot Armed Suspect 10 Times
-
Tech4 weeks ago
Increasing its Stake in OpenAI by $1.5 Billion is a Possibility for SoftBank.
-
Tech3 weeks ago
Canadian Media Firms Are Suing OpenAI in a Potential Billion-Dollar Dispute.
-
Finance2 weeks ago
Chrystia Freeland Promises Mini-Budget By Dec 16th