Every day, hundreds of Canadians hear the difficult news: they have cancer. The latest figures show that cancer cases and deaths are not just rising, but reaching new records in 2024. The Canadian Cancer Society estimates nearly 247,100 new diagnoses and 88,100 deaths this year alone—numbers higher than last year, and a preview of what’s ahead in 2025.
This growing burden touches nearly every family, straining both lives and the healthcare system. Lung, breast, prostate, and colorectal cancers lead the counts, with lung cancer now the top cause of cancer death for both men and women. While cancer rates among older adults drive these increases, cases among younger Canadians are climbing, raising fresh concerns about delayed diagnoses and gaps in screening.
With survivors living longer and new cases on the rise, Canada faces a complex public health challenge. How we respond—through prevention, screening, and support—will shape the future of cancer care across the country.
Recent Epidemiology: Current and Projected Cancer Burden
Cancer isn’t just a story told in statistics—it’s woven into personal lives and communities. The numbers in Canada now stand at an all-time high, and projections show more cases and deaths are on the horizon. Understanding the latest data on incidence, the major types of cancer, and who’s most affected helps paint a clear picture of where Canada stands and what needs attention next.
Canada’s Current Cancer Statistics: Key Data and Trends
In 2024, an estimated 247,100 Canadians will be told they have cancer. That means about 675 people each day get this diagnosis. Cancer will also claim 88,100 lives this year, or roughly 241 deaths daily. These figures are the highest ever seen in Canada and reflect both a growing and ageing population.
While the risk of developing cancer remains high—about 1 in 2 Canadians will face a diagnosis in their lifetime—public health efforts have made progress. Since the early 1990s, the five-year survival rate has climbed to 64% from 55%, thanks to better screening, early detection, and treatments.
Not everything is moving in a hopeful direction. Certain cancers—like liver, melanoma, kidney, and some head and neck cancers—are rising. These increases tie back to risk factors such as alcohol, obesity, hepatitis infections, HPV, and unprotected sun exposure.
Looking ahead to 2040:
- The number of new cases is expected to increase by about 40%.
- Cancer deaths could rise by 44%, mostly because of an older and larger population.
- Healthcare costs for cancer are projected to hit more than $31 billion, up from $20.6 billion in 2020.
Top Cancers by Incidence and Mortality
Some cancers are far more common than others, and a small group causes the majority of cancer deaths. The leading cancers in Canada this year look like this:
New Cancer Cases (2024 projections):
- Lung & bronchus: 32,100 (13%)
- Breast: 30,800 (12%)
- Prostate: 25,700 (10%)
- Colorectal: 24,000 (10%)
Together, these four account for nearly half of all new cases.
Cancer Deaths (2024 projections):
- Lung cancer: 20,700 (23% of all cancer deaths)
- Colorectal: 9,400
- Pancreatic: 6,100
- Breast: 5,500
- Prostate: 5,000
Lung cancer is the main driver in both diagnoses and deaths, more than double the next most fatal cancer. This reflects how challenging it remains to detect early and treat effectively.
Demographic and Regional Disparities
Cancer isn’t experienced the same way across Canada. There are clear differences based on age, sex, region, and even socioeconomic status.
Key disparities include:
- Gender: Men have higher cancer rates and mortality than women. In 2024, men are expected to have an incidence rate of 562.2 per 100,000 compared to 495.9 for women. Death rate follows the same pattern.
- Age: Cancer risk rises with age. Most new cases and deaths are in Canadians aged 50 and older, but rates in younger adults are increasing, especially in types like colorectal and cervical cancer.
- Region: Eastern and Atlantic provinces see higher rates of both new cases and deaths, especially for lung and colorectal cancers. Differences in risk factors (like smoking), access to screening, and healthcare resources play a big role here.
- Socioeconomic status: Lower income or education often links to higher cancer risk and worse outcomes, driven by factors such as reduced access to healthy foods, health literacy, and preventative care.
These gaps show that while progress has been made, not everyone is benefiting equally. Targeted public health actions and policy changes will be crucial to reducing the rising cancer burden across all regions and groups.
Drivers Behind Rising Cancer Cases and Deaths in Canada
No single factor explains why cancer cases and deaths are climbing in Canada. Multiple root causes have collided—from the ageing population to lifestyle habits and deep regional or social inequalities. Understanding what’s fueling these increases makes it easier to act on prevention and close the gaps that leave some groups worse off.
Impact of Ageing and Population Growth
With people living longer and Canada’s population growing, cancer numbers are set to keep rising. Over 90% of cases appear in people older than 50, with the risk climbing further as age increases. The growing number of seniors means more cancer diagnoses year after year.
- Older age brings higher risk: Cells accumulate genetic damage over time, which can lead to cancer.
- Bigger population, more diagnoses: Even if everyone had the same risk, having more people produces more cancer cases.
- Changes in survival: More Canadians are surviving cancer thanks to early detection and better treatment. This adds to the number of people living with or beyond cancer, further squeezing resources.
The increased load from demographic shifts strains not just families, but also the healthcare system, with the cost of cancer care set to surpass $31 billion in the coming years.
Role of Modifiable Lifestyle and Environmental Risk Factors
Lifestyle and environment matter—a lot. Choices we make and exposures we face change our cancer risk. In Canada, these modifiable risk factors are responsible for a large slice of cancer cases.
Some key drivers:
- Tobacco use: Smoking is Canada’s top preventable cause of cancer, used by about 1 in 6 adults. Lung cancer dominates both new cases and deaths because of this.
- Diet, exercise, and weight: Unhealthy eating, too much alcohol, physical inactivity, and excess weight are linked to 30–35% of new cancer cases. These risks often pile up in low-income and rural areas, with fewer options for healthy food or safe exercise spaces.
- Environmental exposure: Carcinogens like asbestos, radon, air pollution, and UV rays from the sun also increase risk. Work settings and region play a role here, with some jobs and places carrying higher risk.
- Infections: Viruses like HPV and hepatitis B or C boost cancer rates for certain organs. Vaccine use and safe health habits help, but gaps remain.
Because these factors can be changed or managed, targeting them with public health strategies holds huge potential to curb future cancer increases.
Socioeconomic, Regional, and Healthcare Access Inequities
Not everyone in Canada faces cancer equally. Where someone lives, their income, and their background play a major part in both risk and outcomes.
- Income and education: Lower-income Canadians carry more risk, in part because they face more barriers to healthy living and healthcare. They may also be more likely to smoke and less able to pay for nutritious food.
- Region and rurality: Some provinces, such as Newfoundland and Labrador or Quebec, ee much higher cancer rates. Rural and remote communities struggle with fewer screening options, longer travel for treatment, and delayed diagnoses.
- Indigenous and immigrant groups: First Nations, Métis, and Inuit peoples and many recent immigrants face higher cancer risks due to unique exposures, lower screening rates, and historic gaps in care. Late-stage diagnoses are more common, impacting survival.
- Systemic gaps in care: Access to timely and appropriate screening is inconsistent. Provinces set different ages and criteria for tests like mammograms or colonoscopies. Wait times and distance to care centres add another centre.
These gaps mean that progress is not shared evenly. Tackling the cancer crisis means paying close attention to the systems that leave certain groups behind, and building pathways so everyone gets timely prevention, screening, and care.
Modifiable Risks and Prevention Opportunities
Cancer doesn’t just arrive out of nowhere. Almost 4 out of 10 cases in Canada could be prevented by making healthier choices and supporting policies that protect health. These preventable risks range from what people eat and drink to where they work and the infections they could avoid. By making even small changes, individuals and communities can lower many cancer risks and help slow the rise in cases and deaths.
Tobacco, Alcohol, Diet, and Physical Activity
Tobacco is still Canada’s top preventable cause of cancer, linked to about 18% of all cases. Smoking accounts for around 86% of lung cancer diagnoses. The fight against tobacco has seen wins, but more than 1 in 6 adults still smoke or use other tobacco products, putting themselves and others (through second-hand smoke) at risk.
Alcohol is another serious but often overlooked factor. Drinking raises the risk for cancers of the mouth, throat, liver, colon, and breast. There’s no safe amount of alcohol—any use can increase risk, and regular or binge drinking magnifies it.
Food choices and movement patterns matter just as much. A diet low in fruits and vegetables, along with too much processed or red meat, adds to cancer risk, especially for colon and stomach cancers. At the same time, excess body weight is a rising problem, now poised to overtake tobacco as the #2 cause of preventable cancers by 2040. Physical inactivity, which often goes hand-in-hand with weight gain, also increases risk.
Key ways to lower risk:
- Stop smoking and avoid second-hand smoke exposure
- Limit or skip alcohol altogether
- Eat more fruits, vegetables, whole grains, and less red or processed meat
- Keep a healthy weight through daily movement and activity
- Make a plan or get support (like quit lines or community programs) for lasting changes
Environmental and Occupational Exposures
Not all risks come from daily habits. The environment at home, outside, and especially at work exposes Canadians to cancer-causing substances.
Common environmental and workplace carcinogens include:
- Asbestos: Still present in many older buildings; linked to lung cancer and mesothelioma
- Radon gas: A leading cause of lung cancer, especially in homes with poor ventilation
- Air pollution: Linked to lung cancer and possibly others
- Ultraviolet (UV) radiation: Causes most skin cancers (from the sun or tanning beds)
- Diesel fumes, chemicals, and industrial solvents: Higher risks for those in mining, construction, factories, and other high-exposure jobs
Some exposures are impossible to eliminate, but they can be made safer through stricter rules, better ventilation, and the use of protective equipment. People can get homes tested for radon, push for safer products at work, and protect their kin by using sunscreen or wearing sun-protective clothing.
Community-level action works best: progress comes faster when cities, employers, and health groups join forces to remove or reduce risks.
Preventive Vaccinations and Infection Control
A few viruses and bacteria are known drivers of certain cancers. The good news? Vaccines and infection control can wipe out almost all cases tied to these germs.
- HPV (human papillomavirus): The main cause of cervical cancer, throat cancers, and some anal cancers. The HPV vaccine, offered to most young people across Canada, can prevent nearly every case.
- Hepatitis B and C: These viruses cause many liver cancers. Vaccines for hepatitis B and screening plus treatment for hepatitis C cut the risk sharply.
- Helicobacter pylori: A bacterium linked to stomach cancer. Treating infections in high-risk groups lowers stomach cancer rates.
Screening and treatment programs, paired with accessible vaccines, can rid future generations of several deadly cancers. Public health efforts now focus on expanding vaccine uptake, removing barriers to care, and making sure no one misses out due to cost, region, or background.
Bottom line: the path to fewer cancer cases is well marked. It runs through individual choices, smarter policy, and credible information—helping Canadians take charge and create safer homes, schools, and workplaces for everyone.
Policy, Public Health Initiatives, and Healthcare Response
Slowing the rise in cancer cases and deaths isn’t only a matter of personal choices—smart policies, strong public health strategies, and evolving healthcare responses shape what’s possible for millions of Canadians. As the numbers grow and patient needs change, every level of government and healthcare works to close gaps, speed up diagnosis, and build fairer systems. Canada’s approach in 2025 reflects fresh thinking, new technology, and a drive to reach every community.
Federal and Provincial Cancer Control Strategies
Canada’s cancer fight draws on long-term planning and innovation at both the federal and provincial levels. The Canadian Strategy for Cancer Control guides national efforts, aiming to cut cancer deaths, improve quality of life, and make care more equitable. Updated in 2019 as a 10-year action plan, it continues to respond to new challenges through:
- Coordinated investment: The federal government works through the Canadian Partnership Against Cancer to unite provinces and territories, aiming for common goals and shared tools.
- Focus on prevention: Strong tobacco control, alcohol policies, promotion of healthy lifestyles, and environmental protections remain top priorities.
- Action on data: Canada’s first Cancer Data Strategy (2023) builds better data-sharing, which helps track progress, close care gaps, and tailor strategies for every region.
- Elimination targets: There’s a dedicated push to eliminate cervical cancer by 2040, expand HPV vaccination, and shift screening to HPV testing. Some provinces now lead in rolling out primary HPV screening, paired with self-sampling options for those missing routine checks.
Provinces remain on the front lines, tailoring policies to local needs. Eastern provinces, struggling with higher cancer rates, get extra attention for prevention, smoking cessation, and screening access, while B.C.’s switch to HPV-based screening is changing the national conversation on what’s possible.
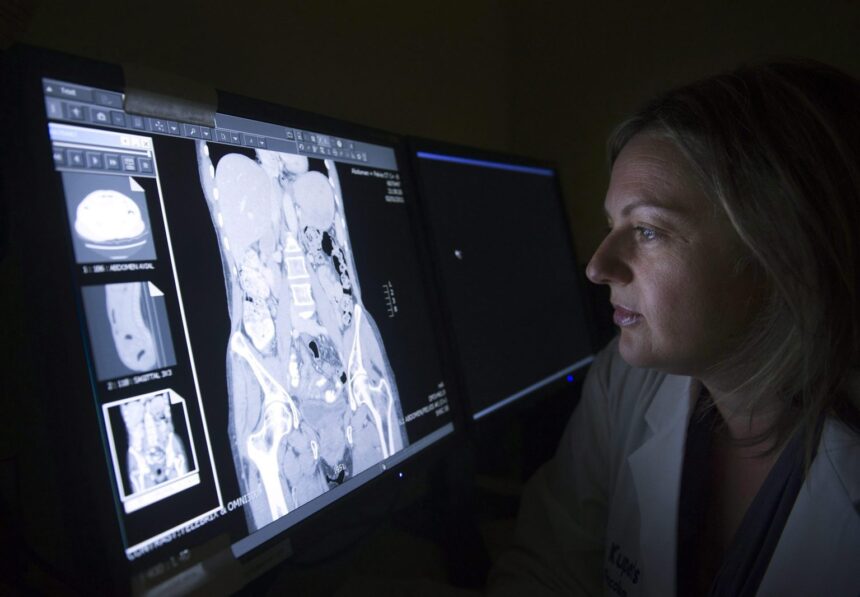
Screening, Early Detection, and Access to Care
Getting ahead of cancer starts with catching it early. Organised screening saves lives, but patchy rules, missed appointments, and long wait times keep Canada from reaching its full potential. Key efforts in 2025 include:
- Lowering screening ages: Advocacy groups pushed for earlier mammograms. Most provinces now allow women to self-refer starting at age 40. Ontario is rolling out HPV-first cervical screening, and there’s mounting pressure to expand colorectal screening to younger groups as early-onset rates climb.
- Boosting participation: The Canadian Cancer Society’s nationwide campaigns raise awareness and make screening reminders more visible. More clinics use digital tools, apps, and virtual visits to catch up with those overdue for tests.
- Multi-cancer early detection: Researchers are piloting tests that check for multiple cancers from a single sample. These complement traditional tests, aiming for faster, less invasive ways to flag disease before symptoms start.
- Closing care gaps: Programs target rural, remote, and Indigenous communities, bringing mobile mammography and stool test kits to more doorsteps. Still, a lack of family doctors and primary care bottlenecks create real barriers, especially for younger people not eligible for standard screenings.
Cutting delays and improving navigation (with patient navigators and rapid-access clinics) help more people move from suspicion to diagnosis without falling through the cracks.
Addressing Equity in Cancer Prevention and Care
Not all Canadians feel the benefit of new technology or policy. Cancer care equity remains a top challenge in 2025, and solutions need to match the diversity of people and places across the country.
- Breaking down barriers: Public health and advocacy groups call out the “screening gap, where low-income, rural, Indigenous, racialised and newcomer populations get diagnosed later and face worse outcomes. Inclusive policies aim to remove language, cost, and geographic hurdles.
- Data-driven approaches: Canada’s new Cancer Data Strategy breaks down cancer rates by geography, income, ethnicity, and experience, highlighting where help is needed most. Localised outreach tailors programs for the realities faced by specific populations.
- Investing in trust and support: Building trust means hiring more diverse staff, supporting cultural safety training, and involving community leaders in care planning. For example, Indigenous-led initiatives and newcomer-specific programs seek to build bridges and reduce fear or stigma.
- Innovating for inclusion: New digital health and ppatient-centredapps apps put appointment reminders, symptom trackers, and information directly in people’s hands. These tools, plus peer-led education and survivor stories, help make cancer care more approachable for those who’ve felt left behind.
A future with fewer cancer cases and deaths depends on everyone getting a fair shot at prevention, early detection, and the very best care. Success rests on action nd accountability at every level.
Conclusion
Cancer touches nearly everyone in Canada, and the rising number of cases and deaths each year is both urgent and personal. This trend shows where attention is needed most: prevention, early detection, and fair access to care for every community.
Progress won’t come from one group alone. Health leaders, governments, community organisers, and everyday Canadians all have a part to play. By working together, it’s possible to close gaps and drive down preventable cancers.
The numbers carry weight, but they are not the end of the story. Investing in healthier choices, stronger screening, and more equal care can save lives. Readers are invited to join this effort, whether by learning more, supporting policy changes, or sharing their stories.
Thank you for caring about this challenge. What would you like to see change about cancer prevention and care in your community? Share your thoughts and help spark the next step forward.