Doctors across Canada have issued urgent warnings as the country’s healthcare system strains under mounting pressure. With emergency rooms stretched past capacity and millions left without a family doctor, even basic care is now harder to get. Families are feeling the impact directly, facing longer waits, rushed appointments, and, in some cases, early discharges from hospitals that desperately need beds.
Physicians say the risk of a system collapse is not just a headline. It’s a real and growing threat that could touch every household, with consequences ranging from delayed diagnoses to higher costs and worsening outcomes. If nothing changes, the cracks in the foundation could widen, leaving patients and communities to bear the brunt. This crisis isn’t limited to overworked hospitals or short-staffed clinics—it affects everyone who depends on timely, reliable healthcare.
Core Problems Driving the Healthcare Crisis in Canada
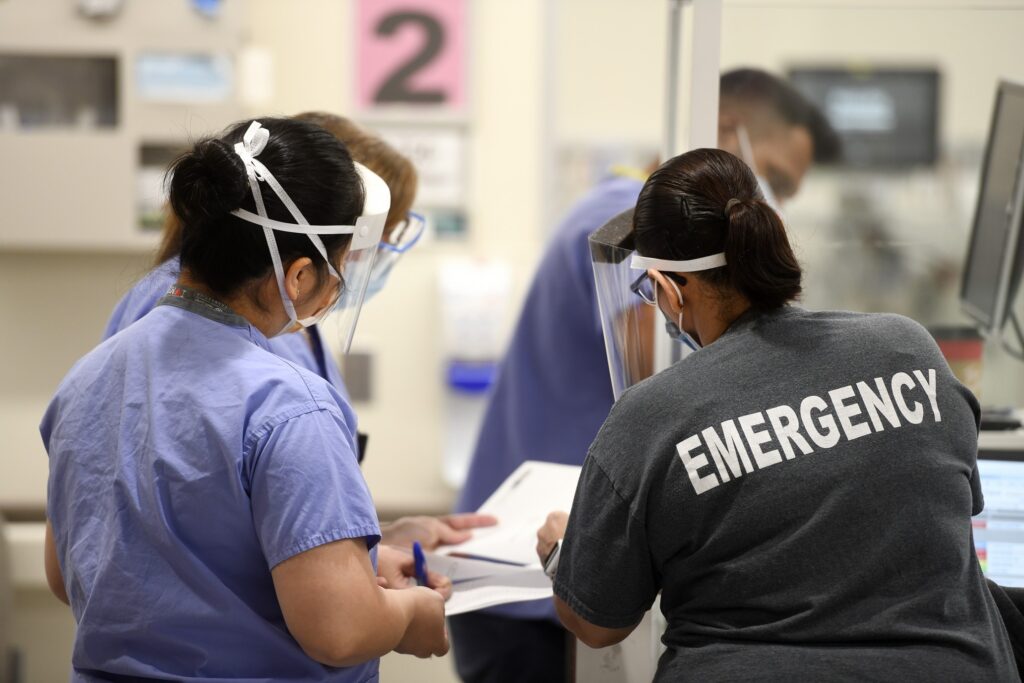
Canada’s healthcare crisis isn’t just about long waits or crowded ERS—it’s about the pressure points squeezing the entire system. From burnt-out staff to millions with no regular doctor, Canadians are feeling the stress at every turn. These aren’t isolated stories—they’re part of a wider breakdown tied to staffing gaps, access issues, and stubborn red tape. To understand how things reached this point, it helps to look at the big challenges head-on.
Staffing Shortages and Overworked Professionals
Hospitals and clinics across Canada face a persistent, severe shortage of healthcare workers. Right now, there are over 78,000 unfilled healthcare positions, according to recent government reports.
This means every day, countless roles for nurses, doctors, and other support staff go unfilled, pushing those who remain to the breaking point. The situation is so dire that the federal government has invested millions to try and attract more professionals, yet the gap keeps growing (Canada allocates $14.3m to attract healthcare workers in 2025).
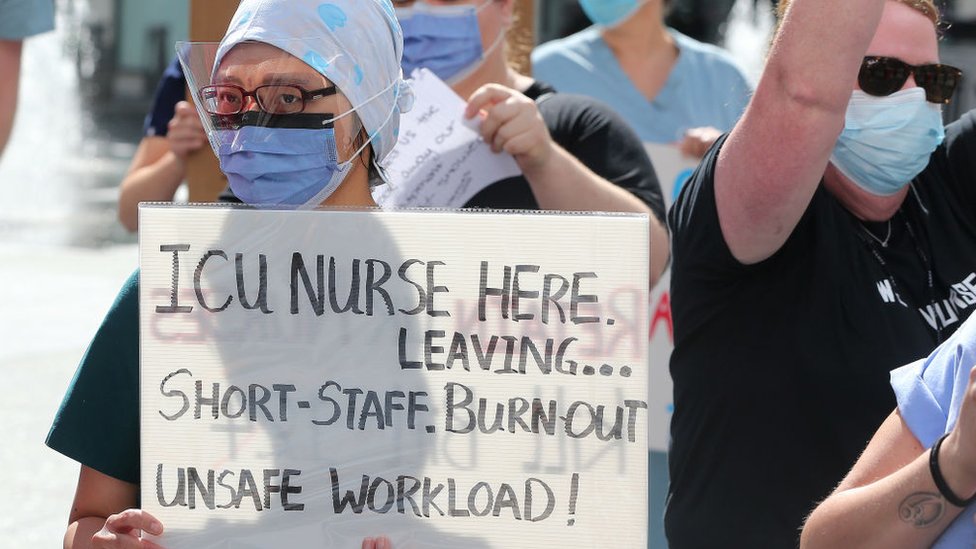
Burnout has spread like wildfire. Many health professionals are clocking in extra shifts, covering for absent colleagues, and dealing with trauma from the pandemic years. Calls for help aren’t new, but the strain is different now—it’s day after day with no relief in sight.
A record number are contemplating early retirement or leaving the field entirely, fueling a cycle of staff loss and even longer wait times. In some provinces, over 90% of doctors say they worry about their clinic’s survival, and more than half are considering quitting or moving.
Barriers to Accessing Primary Care
Millions of Canadians can’t find a regular family doctor. For them, getting simple checkups or timely medical advice becomes a struggle. Recent surveys show that as many as six million people in Canada don’t have a family doctor, and wait times to see a new one can stretch for months. This creates a “haves and have-nots” reality: some get quick, coordinated care, others are left to fend for themselves in overcrowded walk-in clinics and emergency rooms (Canada’s healthcare takes centre stage in 2025 Federal Election).
This gap isn’t just an inconvenience—it’s a serious health risk. Delayed access leads to missed diagnoses, untreated illnesses, and more trips to the ER for issues that should have been managed early. Pediatric and rural patients are especially hard hit. Many have witnessed cancelled surgeries or postponed treatments, while parents worry about children suffering complications that could have been avoided with prompt care.
Administrative and Regulatory Hurdles
Behind the scenes, bureaucracy slows everything down. Hospitals and clinics face mountains of paperwork, funding rules, and regulations that bog down hiring and patient care. Credentialing for foreign-trained healthcare workers is notoriously slow. Many skilled professionals wait months—sometimes years—before they’re allowed to practice, leaving their talents unused during a time of desperate need.
The residency match process for new doctors leaves positions unfilled, while international graduates navigate time-consuming and expensive licensing systems (Unfilled positions after the first iteration of the 2025 R-1 Match). Provinces have different standards and processes, making cross-country movement for staff harder than it should be. All this red tape isn’t just frustrating for workers—it directly impacts patients, leading to bottlenecks, resource waste, and more stories of Canadians left waiting for care.
The crisis is less about a single failing and more about a web of interlocked problems—the answers will require action on every front.
Impacts of the Systemic Crisis on Patients and Providers
Canada’s healthcare system is experiencing more than growing pains—it’s buckling under the combined weight of surging emergency room visits and a crushing backlog for surgeries and basic care. Patients face new barriers almost daily, while providers are left to pick up the slack. The following sections outline the real-world impacts seen across the country, from packed ERS to mounting staff burnout and attrition.
Overwhelmed Emergency Departments and Backlogs
Emergency departments have never felt so crowded. Recent data paints a bleak picture: many ERS now operate far beyond capacity, with patients often waiting half a day (or longer) for care. Hospitals, short on staff and beds, must prioritise only the most critical cases. That means some families spend hours in waiting rooms while their loved ones are triaged, and many who could once rely on fast help now get pushed aside.
It’s not just about ER beds disappearing. The crisis extends to surgical departments and speciality clinics. Countless Canadians are stuck on waitlists that keep growing every year. At some hospitals, waits for elective procedures have stretched from weeks to many months. Delays affecting cancer treatments, joint replacements, and even heart surgeries have led to more complicated health problems and, in some cases, tragic outcomes.
For a deeper dive into this ripple effect, consider a recent review showing that overcrowding in the ER is only the tip of the iceberg. Backlogs for appointments, diagnostic tests, and surgery are creating a new kind of bottleneck, straining every link in the care chain (The great Canadian wait time problem, now with data). In some provinces, the health system is exploring drastic solutions, like converting unused office buildings into healthcare spaces, just to open more beds (repurposing underused office space in hospitals). Overcrowded ERS have become dangerous choke points, with respiratory illnesses and seasonal spikes making everything harder (over-capacity ERS are dangerous choke points).
The result? Many Canadians can’t get care when they need it. As wait times swell and options shrink, the quality of care drops for everyone, from routine cases to life-threatening emergencies.
Mental Health Toll and Professional Attrition
The crisis has flipped the script for healthcare workers. Compassion and dedication alone can’t mask the exhaustion or stress bubbling under the surface. Many frontline staff are working extended hours, often covering for colleagues who are sick or have quit. This grind chips away at well-being, making it harder for anyone to show up at their best.
A recent government snapshot in Ontario found that healthcare providers were increasingly seeking mental health support for anxiety and worry, often triggered by the relentless demands of their job (Ontario healthcare workers sought mental health treatment). Even so, many suffer in silence, pressured to keep going despite the toll.
Among nurses, the numbers speak volumes. In a 2025 survey, just over half rated their mental health as “good” or better, while 14 per cent reported their mental health as “fair” or poor (Mental Health of Nurses in Canada 2025). This persistent strain has direct, real-world costs:
- Increased sick leave and workplace absences
- Rising burnout and professional exhaustion
- Greater numbers are leaving the workforce outright
Burnout is also fueling a wave of retirements and resignations, which feeds the existing staff shortage. Research has found a strong link between burnout and higher turnover rates, with healthcare workers citing the impossible workload and emotional wear as top reasons for leaving (burnout-driven turnover in healthcare).
When experienced staff walk away, both patients and colleagues feel the impact. Newer hires face steeper learning curves, and the remaining team sees their workload swell even further. All of this drives down morale and raises the very real risk of errors, longer wait times, and declining service quality.
Canada’s healthcare system is not only losing expertise—it’s losing hope and stamina. For patients and providers alike, the cost isn’t just measured in time and money, but in health and trust.
How Governments and Stakeholders Respond: Solutions and Reforms Underway
Canada’s healthcare crisis has reached a breaking point. With doctors raising alarms and families waiting longer than ever, the urgency for smart, targeted fixes is clear. The situation is tough, but it’s not without hope. Across the country, governments and healthcare groups have launched new investments, policy shifts, and technology upgrades to steady the system and make care more accessible for everyone.
Federal and Provincial Funding Initiatives
New public investments are being rolled out to expand services, train and hire more staff, and upgrade ageing healthcare infrastructure. Both Ottawa and the provinces have committed extra funds to help hospitals and clinics respond to crushing wait times, staff burnout, and outdated facilities.
- Access Expansion: Funds are being channelled to open new clinics, especially in communities hardest hit by shortages. Targeted grants aim to bring care closer to patients in both rural and urban centres.
- Workforce Growth: In early 2025, the federal government earmarked $14.3 million to recruit and support more frontline health professionals. These investments specifically target gaps in high-demand fields like nursing and family medicine (the Government of Canada is investing up to $14.3 million).
- Modernising Infrastructure: Budget moves in 2025 include funds for renovating hospitals, updating equipment, and expanding digital health tools. This means fewer crumbling buildings and more high-tech care options.
- Mental Health Support: Recognising the toll on healthcare workers, dedicated funding now flows into mental health and wellness programs, aiming to keep providers healthy enough to stay on the job (Health Canada Departmental Plan 2024-2025).
Accelerating Credential Recognition and Leveraging International Talent
One of the smartest ways to ease staffing shortages has been to speed up the process for internationally educated health professionals (IEHPS) to work in Canada. For years, talented doctors and nurses from abroad faced endless paperwork and long waits to get licensed. Now, some overdue changes are happening.
- Faster Licensing: In March 2025, Ottawa announced $52 million in new funding for projects that help foreign-trained professionals get their credentials recognised faster (Foreign Credentials Recognition Program). This focus on efficiency aims to shorten wait times and reduce bureaucratic backlogs.
- Streamlined Pathways: Provinces and territories are rolling out single-window, online applications to cut confusion and make it easier for IEHPs to understand what’s required.
- Balancing Opportunity and Fairness: While quickening the licensing process brings more workers into clinics and hospitals, it also raises tough questions. How do we keep hiring standards high? Can local graduates and newcomers both get a fair opportunity? Stakeholders say these changes must come with strong checks and mentoring built in (New funding for foreign-trained healthcare workers).
These steps won’t fix shortages overnight. But each improvement reduces barriers, taps into untapped talent, and helps hospitals fill jobs that sit vacant month after month.
Digital Health Transformation and Interdisciplinary Teams
To address long queues and patchy service, Canada is investing heavily in digital health tools and expanding the roles of healthcare teams. The push now is to give patients better access, cut redundancy, and help providers move more quickly.
- Interoperable Digital Records: New systems are replacing paper charts, letting doctors and nurses see a patient’s full history with just a few clicks. These upgrades cut errors, save time, and help catch problems early (Canada’s health care crisis demands a digital solution).
- AI and Smart Technology: Clinics are piloting AI tools that help with triage, track symptoms, or flag high-risk patients. These tools promise to scale care and spot trends before they become emergencies.
- Expanding Provider Roles: Interdisciplinary teams—like nurse practitioners, pharmacists, and therapists—are taking on more responsibilities. When these providers work together, patients get quicker care, and doctors can focus on the most complex cases.
- Patient-Centred, Equitable Care: These changes aim to put patients at the centre. With digital access, people can check their records, book visits, and ask questions online, cutting wait times and travel, especially in remote areas (The Future of Digital Health in Canada).
The road ahead is still challenging, but government action and smart innovation are offering a way forward. Each new step, from funding to tech upgrades and smarter credentialing, chips away at the barriers standing between Canadians and the timely care they deserve.
The voices of doctors across Canada make it clear: patchwork fixes will not be enough to stop the healthcare system from sliding deeper into crisis. Even as governments boost funding, modernise technology, and seek more talent, especially from abroad, access remains uneven, and wait times keep rising.
At the heart of the matter are exhausted staff, overloaded clinics, and patients falling through the cracks. Solutions are underway, but nothing short of steady, countrywide action will give Canadians the secure, timely care they expect.
What’s at stake is the health of families, trust in public care, and Canada’s promise of universal coverage. Sustained focus and open collaboration among all stakeholders are needed next, not just for recovery, but to give everyone a fair shot at a healthy future.
Canadians count on their healthcare system. Now, it’s up to leaders and citizens alike to keep it strong. Readers are encouraged to share their stories and ideas on how we can build a better path forward, because the system touches everyone. Thanks for staying informed and being part of the solution.